




Summary
Did you know that when we say a child has an attachment disorder, it is often not the whole picture? It is only one part of a seven-piece jigsaw puzzle called ‘developmental trauma’. By putting together the puzzle, we can understand how a child’s adverse childhood experiences have shaped their emotional world and outward behaviour. Once we understand this, we can then work with a child to help them with their developmental trauma using an innovative therapeutic approach called the ‘Neuro-Sequential Model of Therapeutics’. This model recovers and repairs each part of a child’s brain in a specific, phased and effective order. We need to ensure that the child’s different environments work together using this model as a whole; including home school, therapy and even the GP – to ensure the child’s best chances for recovering from their trauma and loss. Developmental trauma can be repaired – if we get the order and type of support just right.
Attachment is adaptive
The ideas described here are a holistic and whole life approach designed to help a child and their parent/carer to recover and repair from early trauma and disrupted attachment. It is an approach based on cutting edge research, and can be applied by everyone who knows a child who has been through chronic stress or repeated trauma.
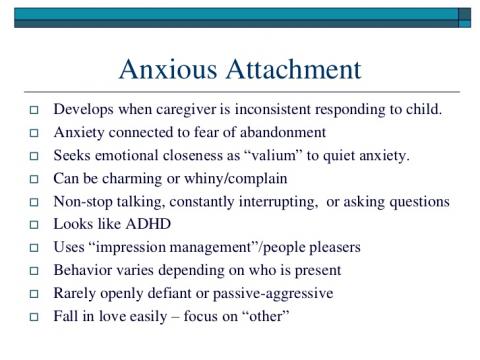
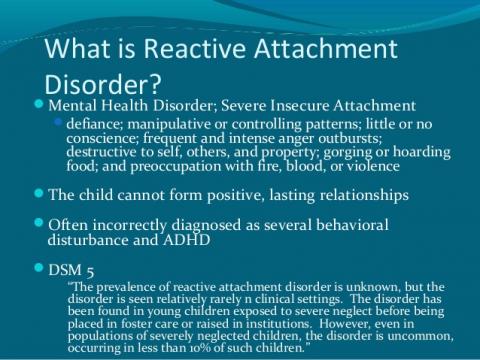
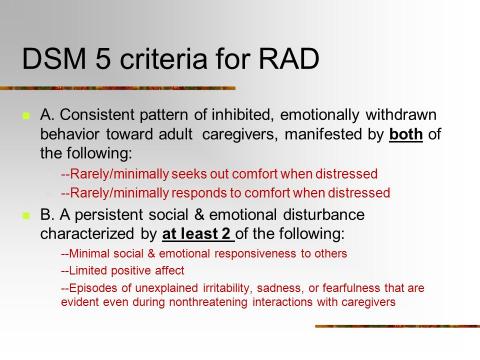
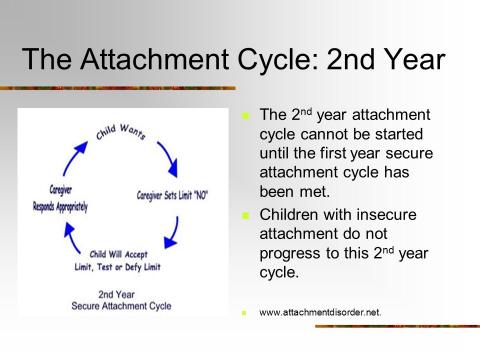
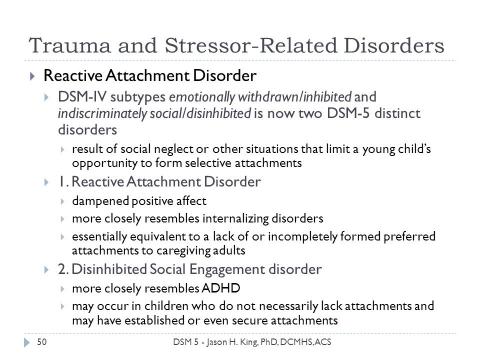
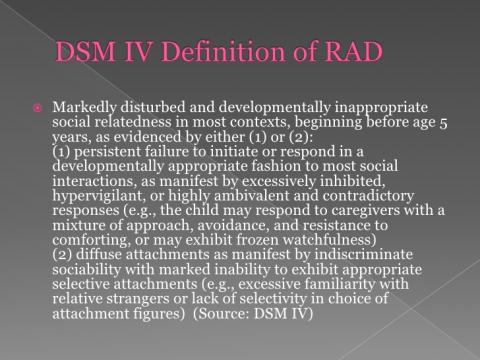
The majority of people immersed in the world of working with or caring for vulnerable children have been taught about attachment styles. They understand the idea of ‘insecure attachment’ and that a child will either be ‘insecure avoidant (disconnected), ambivalent (highly emotional and resistant) or disorganised in their attachment. This is the child’s best way of coping with threat and danger.
Psychologist, Dr Patricia Crittenden, has now provided us with a heavily researched modern attachment theory that helps us take this further.
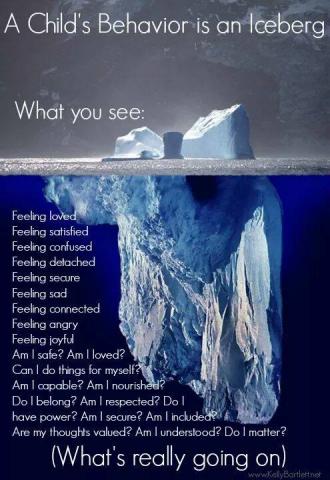
Crittenden has shown us that frightened children are not actually disorganised in their behaviour, but in fact they always organise themselves around danger by using a fluid combination of attachment behaviours to survive the environment they are in at that given moment. Children often have a ‘default’ attachment pattern, but they do not have one static attachment style. This helps us to understand why many vulnerable children are shut down (seen as “good”) at school yet fall apart at home; or vice versa. It also helps us to understand why it can be so hard for some professionals to really see what is going on in a child’s emotional world, as vulnerable children are so incredible at adapting to their environment.
But is attachment theory enough?
We (parents and professionals) have been so focussed on attachment that the other six pieces of the jigsaw puzzle are often not appreciated nor addressed. Without putting all these pieces together, working with a child who has early trauma is less likely to be effective and more likely to compound feelings of shame and inadequacy and ultimately failure.
Developmental Trauma
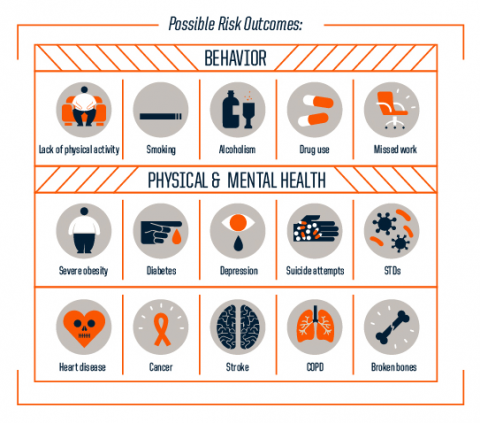
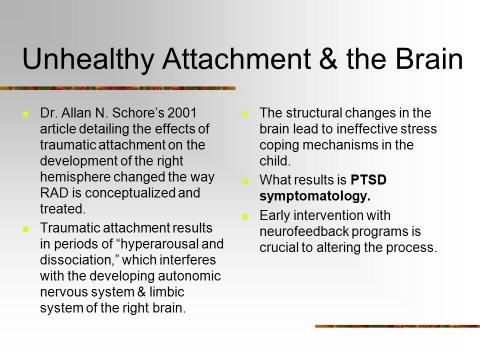
Children who have had a one off single traumatic event will likely show signs of PTSD. Children who have had multiple early life traumas will show symptoms of developmental trauma – which is a set of profound problems in all areas of their development.
It is becoming apparent that parents, teachers and therapists are not always aware of the other six jigsaw pieces which are just as severely impacted as attachment. Psychiatrist, Bessel Van der Kolk, has taught us that Developmental Trauma includes the following areas of difficulty:
When supporting a child with developmental trauma in therapy or in school, it is important to consider each and every one of these areas of impact.
Repairing from the bottom up
Hundreds of studies have shown us that children who suffer many adverse life experiences essentially suffer damage to brain development. As their brain grows, the negative impact on their neural systems means their brain is impaired and does not function as it should do. Considering it this way – a child suffering a ‘prolonged brain injury’ across the time that they are in a toxic environment – is more accurate than thinking that of their problems as simply ‘insecure attachment’.
Bruce Perry, a pioneer psychiatrist in the area of child abuse and neglect, has developed what is known as the Neuro Sequential Model of Therapeutics. Perry reassures us that developmental trauma can be repaired, BUT it depends on the nature, sequence, timing and duration of the support. In other words, trauma repair can happen only if treatment (and parenting/schooling) is organized in the order in which the brain injury needs to heal.
Even the best therapy will not work if we start in the wrong place and at the wrong time for that child.
Here’s what you need to know about repairing developmental trauma in a way that is more likely to create change for the child:
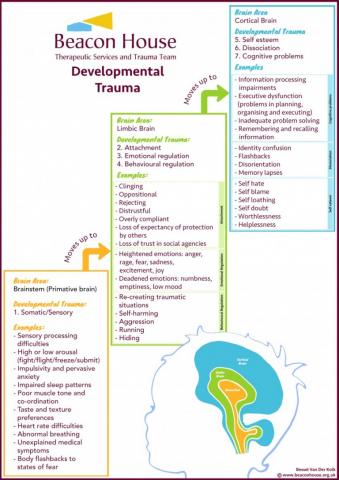
The brain is organised in a hierarchical way. Here is the order that the brain develops as the child grows from birth to adolescence:
1. Motor and sensory input (brain stem/mid brain)
2. Attachment, emotions and behaviour (limbic brain)
3. Thinking, planning, inhibiting & learning (cortical brain)
The brainstem – the primitive part of the brain – is responsible for keeping us safe. It is the part of the brain that makes us run away from danger, fight for our life or freeze inside; and it keeps us alive. This is very helpful for a child living in a dangerous environment. Their brainstem will constantly be on high alert, ready to keep them safe and to prevent danger. It does its job extremely well.
The problem for traumatised children is that when they transition into a safe environment, the primitive brain does not turn off, so the child stays continuously in survival mode. We see these children operating constantly in Fight/Flight/Freeze/ mode; and normal every-day events signal danger to their brain. The child is developmentally stuck in their brain-stem, very little information can get passed up to the higher parts of their brain. Whilst they are stuck here, they cannot form secure attachments; manage their emotions or behaviour; think, learn or reflect because they are simply trying to stay alive in a world that they feel is highly dangerous. The key message here is that children’s brains develop from the BOTTOM UP, and the higher brain regions do not work properly if the lower brain regions are stuck.
Academic learning happens in the cortical brain. If proper development in the first two brain areas does not happen, the child will not be able to learn, no matter how good the teacher is!
The child cannot form secure attachments and cannot think and reflect, because their brain is stuck on a loop in the brain-stem, illustrated in the Survival Loop diagram below.
Implications for therapy, education and parenting:
1. Everyone in a child’s life needs to be aware of and understand the full picture of Developmental Trauma: A brain injury that needs a ‘whole environment’ approach to repair it.
2. The first goal of any intervention plan needs to be to stabilize the child’s home and school environment, and to regulate their brain-stem.
3. The child’s primary carer – whether that be birth parent, foster carer, adoptive parent or family member – needs support and nurture from their network. Without first a safe base at home, no amount of intervention outside of the parent-child relationship will be effective. This is a crucial part of stabilization.
4. We must look after the parent/carer by addressing their mental health and secondary trauma needs. Caring for a child with developmental trauma is difficult in all aspects of life, and will naturally trigger buried issues in the adult. These need to be supported and the parents’ brain repaired so they can help the child repair. The parents’ mind needs to be the child’s safe base. Sensitive parenting calms the child’s fear over time.
5. The ‘challenging behaviour’ we see in the child begins in the brain-stem, the primitive brain. Without addressing the developmental needs of the brainstem, the other parts of the brain will remain virtually immune to treatment. Traditional talking therapies usually do not work with children who have brain injury to their brainstem as they simply cannot process cognitive conversations, or develop ‘insight’. It can even make things worse as the child will feel a failure for not being able to do something their brain isn’t developed enough to do anyway.
6. Traditional parenting does not work so well for children stuck developmentally in their brain-stem either. Parents/carers need to be trained in a unique approach to parenting therapeutically, to enable the child to regulate their senses; before attachment can become more secure; and before the child can make sense of their life story.
7. Children with brain-stem hypervigilance, impulsivity, and anxiety need patterned, repetitive activities to re-organize and regulate the brain-stem. This includes dance, drumming and music. Eadaion Breathnach (an Occupational Therapist) has developed the innovative and pioneering approach known as Sensory Attachment Intervention. SAI is a trauma-informed sensory processing therapy which calms the fear response in children; and re-attunes the relationship between the child and adult. Sensorimotor Psychotherapy and drama therapy are other body based approaches that work specifically ‘bottom up’. Such body/sensory work should be offered first to enable the child to benefit from traditional talking therapy later in their therapy journey.
8. Brainstem-activities need to be consistent, predictable, patterned and very frequent, over a sustained period of time. This is what it takes to re-train the brain-stem. This needs to be mastered first, before the child is expected to sit and think, reflect and learn. Attachment-focussed interventions focussed on re-training the limbic brain also need to be consistent, predictable, frequent and sustained. Change takes persistence and time.
9. Parenting, schooling and therapy needs to be offered bottom up – teaching the brainstem first, then the limbic brain and finally the cortical brain. Different treatments and approaches are suitable for the different areas of brain repair. Knowing what which part of the brain you are trying to re-train and repair means you can focus your support accurately.
10. Parenting, schooling and therapy need to be emotionally and socially matched, not age matched. Children do not of course move between their brain’s developmental stages in a neat sequence, in fact they move back and forth between the brain areas as they mature. A traumatised child who is able to think and reflect for most of the time can however be triggered into his or her brain-stem survival mode very easily. The key is to respond the child’s developmental age in that moment.
11. Each child is unique and so is their brain. Any therapeutic plan should be generated once it is clear which part of the brain the child is mainly operating from. There is no ‘one size fits all’. A trauma-informed psychological assessment can identify what the child’s support needs are and is essential to map the territory of treatment.
12. Early intervention is crucial. The brain is developed 90% by the age of 4, so early help is essential for repair. When considering a Child Looked After, intervention using this approach should be used as soon as a child has been removed from their birth parents. By waiting for a crisis we will significantly prolong and worsen the effects of trauma on the brain. Life story work when the child is still learning to tame their brainstem or develop attachment will be at best unsuccessful, and at worst harmful.
13. The child – like an adult – is a complex being made of many different parts and therefore the assessment and interventions offered need to touch every part of the child’s life. Home, school, therapy and the child’s support network MUST work together for an effective treatment for the child’s trauma; to enable the child to meet their developmental milestones. A multi-disciplinary approach is a must.
14. Each person working with the child needs to have a safe, regular, consistent and healthy relationship. Humans are designed to exist in close relationships and tight communities!
At Beacon House Therapeutic Services and Trauma Team (www.beaconhouse.org.uk) we base our assessments and intervention plans on the neuro-sequential model of therapeutics. We see therapy for traumatised children as a long-term, holistic, phased approach. An example of how we apply the model to our treatment planning for each area of brain development is as follows:
The profound impact for all children if we used this model in all landscapes could be life-changing. Download this information sheet to share with others connected to a vulnerable child, and ask the question: what can you do differently based on this scientific approach that could start to make a real difference?
All the diagrams and the article itself can be individually downloaded here and used as training resources. Please credit ‘Dr Shoshanah Lyons, Beacon House Therapeutic Services and Trauma Team’ when using these as training materials
WATCH THE ANIMATION VERSION OF THIS ARTICLE HERE.
Dr Shoshanah Lyons is a Clinical Psychologist and Clinical Director of Beacon House Therapeutic Services and Trauma Team, West Sussex. Email Dr Lyons at: s.lyons@beaconhouse.org.uk
With thanks and credit to:
Bruce Perry, Bessel Van der Kolk and Patricia Crittenden for their original work on Developmental Trauma, Attachment and the Neuro Sequential Model of Therapeutics.